NM Medication Administration Record free printable template
Show details
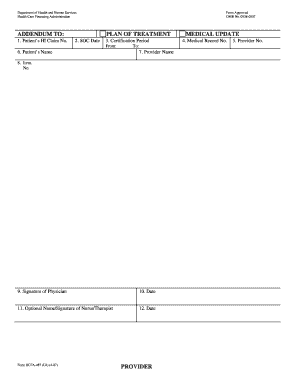
MEDICATION ADMINISTRATION RECORD. MEDICATIONS. HOUR 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 ...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign paper mar form

Edit your mar printable form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your pdffiller form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing paper medication administration record online
Follow the steps below to benefit from a competent PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit record administration form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Create an account to find out for yourself how it works!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out printable medication administration record template word form

How to fill out NM Medication Administration Record
01
Begin by identifying the patient for whom the medication is being administered.
02
Write the patient's name, date of birth, and medical record number at the top of the form.
03
Enter the date of administration in the designated space.
04
List all medications being administered, including dosage, route, and frequency.
05
For each medication, indicate the time administered and any observations or reactions.
06
Sign your name and provide your title or position.
07
Ensure the record is complete and accurate before submitting or filing.
Who needs NM Medication Administration Record?
01
Nurses administering medication to patients.
02
Healthcare providers involved in patient care.
03
Facility administrators for record-keeping and compliance.
04
Pharmacists reviewing medication administration records.
Fill
fillable medication administration record
: Try Risk Free






People Also Ask about mar medical abbreviation
How do you document medicine on Mar?
The times and dates the medication is to be taken 3. The initials of the person assisting with the medication 4. A start date should be noted; a stop date is noted when known 5. Identifying information about the individual, including date of birth, allergies, diagnoses, and names of medical providers.
What are Mar sheet codes for?
At the bottom of every MAR sheet there are several codes relating to medication administration. These are used to indicate what happened when the medication was administered.
How do you write a mar chart?
MAR charts must be clear, accurate and up to date. A MAR chart should contain the following information: Patient details: -Full name, date of birth and weight (if child or frail elderly) and include known allergies and type of reaction experienced.
What are the codes on a MAR chart?
Our cheat sheet R = Refused. When a service user refuses a medication. T = Taken. When a medication is consumed by a service user. NT = Not taken. ADM = Administrated by. WT = Witnessed by. C = Hospitalised. D = Social leave. E = Refused and destroyed.
What should the Mar include?
A MAR includes key information about the individual's medication including, the medication name, dose taken, special instructions and date and time.
What type of information is recorded on a Mar?
The Medication Administration Record (MAR) is used to document medications taken by each individual. A MAR includes: 1. A column that lists the names of medications that are prescribed 2.
How do you make a medication administration record?
The times and dates the medication is to be taken 3. The initials of the person assisting with the medication 4. A start date should be noted; a stop date is noted when known 5. Identifying information about the individual, including date of birth, allergies, diagnoses, and names of medical providers.
Why do you need a MAR chart?
Purpose of the MAR chart: MAR charts are the formal record of administration of medicine within the care setting and may be required to be used as evidence in clinical investigations and court cases. It is therefore important that they are clear, accurate and up to date.
How do you make a MAR chart?
A Formal Confidential Record of Medication Administration. MAR charts must be clear, accurate and up to date. A MAR chart should contain the following information: Patient details: -Full name, date of birth and weight (if child or frail elderly) and include known allergies and type of reaction experienced.
What should be included in Mar?
The MAR chart is clear, indelible, permanent and contains product name, strength, dose frequency, quantity, and any additional information required.
How do I get a Mar chart?
MAR charts in domiciliary care or community care may sometimes be supplied pre-printed by community pharmacies or produced by the care provider with assistance from a pharmacy.
What are the 3 checks of medication administration?
7 Rights and 3 Checks of Medication Administration The right medication (drug) The right dose. The right route. The right time.
What is the correct process for completing a handwritten mar?
General principles be legible. be signed by the care home staff or care workers. be clear and accurate. have the correct date and time (either the exact time or the time of day the medicine was taken) be completed as soon as possible after the person has taken the medicine. avoid jargon and abbreviations.
Where can I get a mar sheet?
Some pharmacies may provide MAR sheets; one can also prepare a handwritten MAR sheet.
What is the correct process for medication administration?
There are five stages of the medication process: (a) ordering/prescribing, (b) transcribing and verifying, (c) dispensing and delivering, (d) administering, and (e) monitoring and reporting.
When should you document the administration of a medication?
NEVER document that you have given a medication until you have actually administered it. 3. The label on the medication must be checked for name, dose, and route, and compared with the MAR at three different times: When the medication is taken out of the drawer.
How do you record on a Mar chart?
MAR chart for domiciliary care The name and date of birth of the person being cared for. The name, strength and formulation of the medicine/s. How often or the time the medicine should be taken. How the medicine is taken or used (route of administration) The name of the person's GP practice. Any stop or review date.
How do you document a Mar?
The following are examples of information to include on the MAR: Month and year that the Medication Administration Record represents. Date order was given, and date and time medication was administered. Initial of the person transcribing the order. Initial of the person giving the medication.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the mar chart template electronically in Chrome?
Yes. By adding the solution to your Chrome browser, you can use pdfFiller to eSign documents and enjoy all of the features of the PDF editor in one place. Use the extension to create a legally-binding eSignature by drawing it, typing it, or uploading a picture of your handwritten signature. Whatever you choose, you will be able to eSign your medication administration record in seconds.
How do I edit medication administration template on an iOS device?
You certainly can. You can quickly edit, distribute, and sign mar sheet pdf download on your iOS device with the pdfFiller mobile app. Purchase it from the Apple Store and install it in seconds. The program is free, but in order to purchase a subscription or activate a free trial, you must first establish an account.
Can I edit printable mar sheet on an Android device?
You can edit, sign, and distribute mar sheet example on your mobile device from anywhere using the pdfFiller mobile app for Android; all you need is an internet connection. Download the app and begin streamlining your document workflow from anywhere.
What is NM Medication Administration Record?
The NM Medication Administration Record is a documentation tool used in healthcare settings to track the administration of medications to patients.
Who is required to file NM Medication Administration Record?
Healthcare professionals, particularly nurses and pharmacists, are required to file the NM Medication Administration Record whenever medications are administered to patients.
How to fill out NM Medication Administration Record?
To fill out the NM Medication Administration Record, one must record the patient's name, the medication administered, dosage, time of administration, and the signature of the person administering the medication.
What is the purpose of NM Medication Administration Record?
The purpose of the NM Medication Administration Record is to ensure accurate tracking of medication administration, enhance patient safety, and provide a legal record of medication use.
What information must be reported on NM Medication Administration Record?
The information that must be reported on the NM Medication Administration Record includes the patient's name, medication name, dosage, time and date of administration, route of administration, and the signature of the healthcare provider.
Fill out your NM Medication Administration Record online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Mar Sheet Template is not the form you're looking for?Search for another form here.
Keywords relevant to printable printable medication mar sheet
Related to med pass sheet
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.